Part 1: Non-Machine Based Assessments
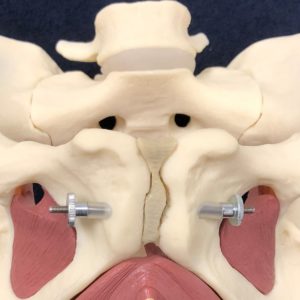
Pelvic floor muscle (PFM) strength is important for various reasons, such as the prevention of urinary incontinence. Your PFM’s are made up of two layers, your superficial PFM’s and your deep PFM’s. A PFM contraction involves a combination of a squeezing action of your superficial muscles and a lifting action of your deep muscles. A PFM contraction has a contraction and a relaxation phase, to which both are equally as important. This contraction becomes a four step process:
 1. Superficial muscles squeeze/tighten
1. Superficial muscles squeeze/tighten
2. Deep muscles lift
3. Deep muscles lower
4. Superficial muscles release
It is the coordination and strength of these muscles that ensure their effectiveness. There are a number of ways to objectively assess the function and integrity of your PFM’s. These include both machine and non-machine based assessments. Today we will be discussing non-machine based assessments which include digital assessments, perineal observation and hiatal assessment.
Digital assessment refers to a single or two finger internal examination of the PFM contraction. From this, the assessor can utilise scales such as the Brink Score, Modified Oxford Scale or the new ICS 4 Point Scale to try and quantify the woman’s PFM contraction. These scales grade the PFM contraction based on the strength of the contraction. For example, comparing a ‘flicker’ of the muscles to a moderate contraction against resistance. This can then be used as a reassessment to track the woman’s improvement. However, evidence suggests that due to the use of these scales being heavily subjective in nature that it is unreliable to rely on these in isolation as being able to truly quantify a woman’s PFM strength. In addition, the ability to contract your PFM’s is but one component in determining if a pelvic floor is functional and this may not be very helpful when it comes to assessment of Prolapse (descent of internal organs).
Perineal observation refers to the location of the Perineum relative to the Ischial Tuberosites (more commonly known as your ‘sit bones’). This is measured on both PFM contraction and on valsalva (bearing down). On PFM contraction, the Perinuem should be lifted up away from the Ischial Tuberosities. According to Grimes et. al. 2012, abnormal perineal descent is diagnosed when the Perinuem is greater than or equal to 2cm below the level of the Ischial Tuberosities on valsalva. Perineal observation can be helpful in determining how supportive your pelvic floor is both at rest and during functional tasks. However, there is limited research to back up the reliability and validity of this assessment at this stage.
Hiatal Assessment can also be used to assess the function of your PFM’s. This assessment can be split up into assessing the size of the Genital Hiatus which is referring to the superficial PFM’s and the size of the Levator Hiatus which is referring to the deep PFM’s. This is usually assessed at rest and on valsalva. By performing a Hiatal Assessment, it can give a better understanding as to how well your PFM’s are supporting your internal pelvic structures such as your organs. Research has shown that greater Hiatal size can be associated with a woman more likely to suffer from Prolapse, a worsening stage of Prolapse and Prolapse surgery failure rates. Vaginal Births are shown to result in a larger Hiatal size and therefore a Hiatal assessment can be very beneficial postnatally to ensure appropriate recovery and return to exercise.
Here at Bend + Mend, we use all of the above assessments together to ensure the optimal assessment of PFM function. In addition, machine based assessments are also performed but this will be discussed in my next blog in more detail. If you are uncertain about how good your PFM function is then come and see Bonnie, our Women’s Health Physiotherapist at Bend + Mend Physiotherapy in Sydney’s CBD.