Sciatic nerve pain is a common complaint with 1 in 10 people experiencing an episode of lower back pain in their lives and 20-30% of those people suffering sciatic symptoms or referred pain down the leg, potentially all the way to the toes.
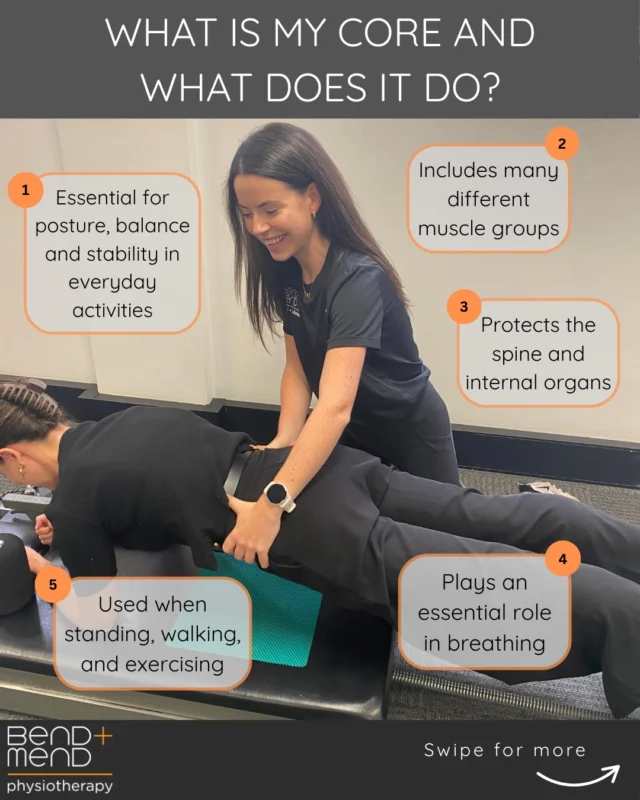
The sciatic nerve runs a tricky course within the pelvic space. It originates from the lower spine branching from the L3-S1 spinal levels. It then travels through the deep gluteal space via the great sciatic notch. In 90% of the population it then tracks underneath the piriformis muscle. In 7% the sciatic nerve passes through the piriformis muscle belly.[1] From there it travels over the deep pelvic muscles – obturator internus and gemelli complex- to exit the pelvic area via the ischial tunnel.
This may sound complex, and it is! There are many structures which can interrupt the course of the sciatic nerve.
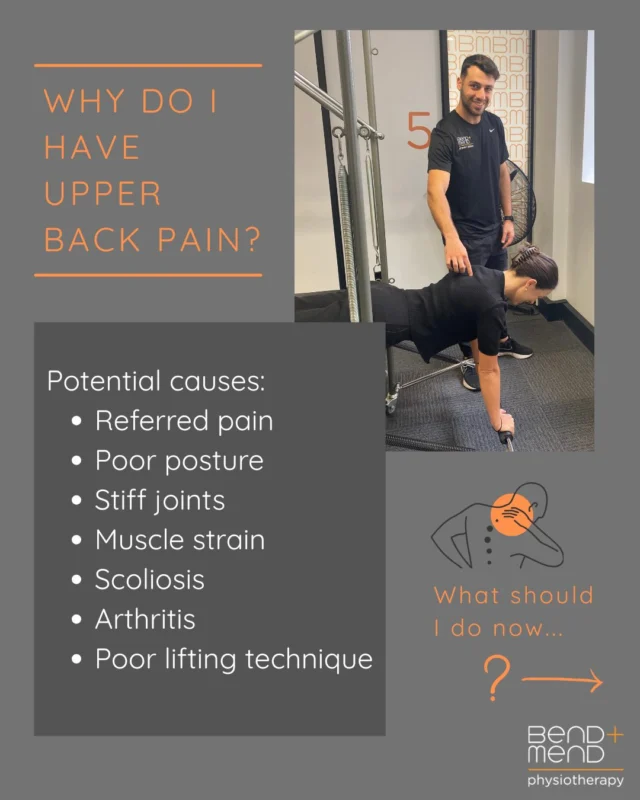
Inflammation or pathology can arise from discs within the spine, causing nerve root compromise. Other pathology can arise due to its tricky pathway along the track. The nerve can become irritated or ‘impinged’ by the adjacent structures deep beneath the gluteus maximus. Both presentations can cause patients pain at the site of impingement and/or symptoms along the course of the nerve.
Sciatica or sciatic nerve pain is diagnosed mainly through a thorough history and physical exam. Commonly patients are asked to describe the distribution of symptoms as it radiates down the leg. Neurological testing such as strength, sensation and reflexes are also helpful in diagnosing between nerve root compromise or irritation of the nerve further down its path. Imaging can be indicated for patients who have severe symptoms, not improving with conservative physiotherapy management or in patients whose symptoms clinically indicate disc herniations, spinal changes and other more severe pathologies.
A condition which can cause sciatic symptoms is ‘piriformis syndrome’ a highly documented, overly diagnosed cause of irritation. Studies have recently been discussing the relationship between the sciatic nerve and the deep hip external rotators and how other sites along the course can cause ‘irritation’ or sciatic symptoms.
A thorough clinical exam is essential in detecting the cause of symptoms and as a result the best rehabilitation approach. It is certainly not a one shoe fits all approach that will help individual complications leading to sciatic pain referral.
If you have been struggling with back pain either on-going or acute with changes such as pain, strength or sensation, nerve type shooting pain or pins and needles observed down the leg then come on in and see one of the team here at Bend + Mend.
Reference:
[1] Koes, B. W., van Tulder, M. W., & Peul, W. C. (2007). Diagnosis and treatment of sciatica. BMJ (Clinical research ed.), 334(7607), 1313–1317.



Hi Lauren
After 3 years of WFH, the ache in my left buttock was initially diagnosed as a Piriformis issue.
When it worsened, my GP sent me for an X-ray which indicated that there were osteophytes or bone spurs at L4-L5.
Stretching, bending and swivelling my hips has not been able to alleviate the now constant ache.
What do you recommend? (Please do not suggest that I visit a physio 🙂 ) Thank you.
Hi Pauline,
Thank you for replying to this post. As I’m sure you read, your symptoms could be a result of multiple factors. It may not be that mobility is your issue but rather a strength issue (loss of strength) which affected many of us during the COVID work from home lifestyle change. There also could be some contribution of lumbar spine pathology which may be contributing to these symptoms for you. That being said it is impossible to give you any more helpful or specific advice without an thorough assessment which would dictate our diagnosis and management of your symptoms. A constant ache should not be your new normal! I would suggest (even though you told me not to!) that a full assessment by a GOOD physio of your lumbar spine and hip would be the next step for you in diagnosing and establishing a treatment plan to reduce your pain and long term symptoms. We’d be more than happy to help you out so please get in touch if you have a change of heart. Best of luck with it all!