Overactive Bladder (OAB) is one of the most common conditions that presents to Women’s Health Physiotherapists. The International Continence Society (ICS) defines OAB as an increase in urinary urgency usually associated with increased frequency of urination with or without incontinence that occurs in the absence of infection or other pathology.
The urge to urinate occurs when our bladder (which is lined with a muscle called the detrusor) expands to an increase in volume of filling urine. When a certain level is reached (usually about 400mls) a signal is sent from the bladder to the brain that it’s time to go to the toilet. When it is convenient and we are sitting on a toilet, the brain sends a signal for the detrusor muscle to contract and the pelvic floor muscles to relax and we can begin to urinate.
Historically, the increase in need to urinate was thought to be a symptom of over-activity in the detrusor muscle sending more “need to pee” signals to brain. So even when the bladder was not full, signals were telling the brain it was time to go. However, this view of over active bladder and increased urination might be overly simplistic. New research has broadened our understanding of OAB and given better tools for treatment and education.
Research by Dr Rebekah Das has elaborated that urgency has multiple influences that come from physiological, biological and environmental inputs. Evidence shows that centralization (an increased sensitivity of the nervous system) can occur in people with OAB. This means that patients with chronic OAB can experience neurological changes in the brain and spinal cord that make them more sensitive to signals that stimulate detrusor activity. For example, the sound of rushing water can make most of us think of heading to the loo but, for someone with OAB, can trigger a much stronger response and need to go. As the nervous system gets more sensitive to signals the more easily the bladder is triggered to send those “need to go” signals even when not full.
Part two looks at how this research is helping treatment of urinary urgency.
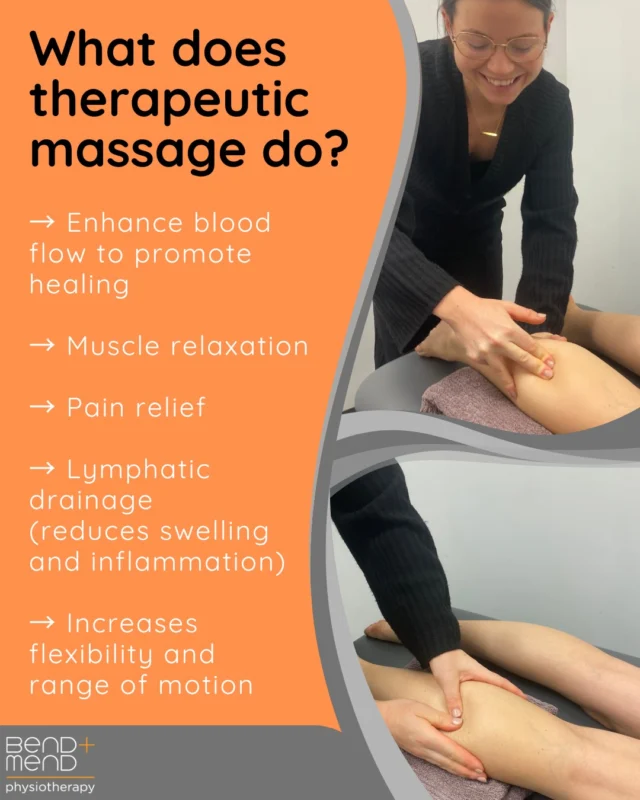
Here at Bend + Mend our Women’s Health Physio has specialised training in the management of conditions such as OAB.
References:
- Loeser JD, Treede RD. The Kyoto protocol of IASP basic pain terminology. Pain 2008;137: 473–7.
- Das, R. (2014). Characterisation of the sensation ‘desire to void’ in individuals with and without overactive bladder. School of Health Sciences, University of South Australia, Doctor of Philosophy.