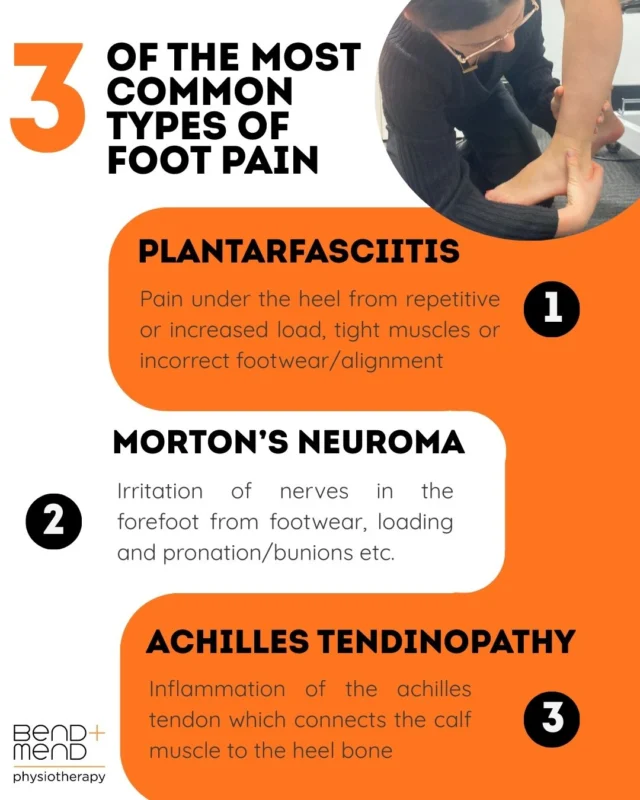
Have you ever had that lingering foot pain that doesn’t seem to ease? This post will cover three common causes of foot pain including plantarfasciitis, Morton’s neuroma and achilles tendinopathy and how physiotherapy can help.
Our feet are remarkably complex structures designed to bear weight, absorb impact, and provide balance and propulsion to aid with gait and other daily functional tasks. There are many different joints in the foot, all with their own respective purpose, function and unique features. Foot pain is a frequent reason people seek physiotherapy care. Whether presenting as sharp heel pain when you take your first steps in the morning, burning sensations in the forefoot, or diffuse aching after prolonged standing, understanding the source of pain is crucial for effective treatment. This blog will explore several common causes of foot pain and discuss how physiotherapy advice and treatment can help promote recovery, improve function, prevent re-occurrence and get you back to doing the things you love quicker!
Plantarfasciitis
Plantarfasciitis is one of the most prevalent causes of heel pain, accounting for a significant proportion of foot related presentations in physiotherapy practice. Plantarfasciitis occurs in about 10% of the general population. It involves inflammation, or in some cases micro-tearing, of the plantarfascia, a thick band of connective tissue that supports the arch of the foot and connects the heel bone (calcaneus) to the toes (phalanges).
Common causes of plantarfasciitis include:
- Repetitive overloading such as running, prolonged standing and walking.
- Poor footwear with inadequate arch support. This means the plantarfascia can get inflamed due to poor resting mechanics.
- Reduced dorsiflexion or tight calf muscles can cause an imbalance in the foots mobility.
- A sudden increase in training load or intensity. This relates to the first point outlined where the plantarfascia is exposed to load that it perhaps is not appropriately conditioned for.
- Foot posture abnormalities such as flat feet (pes planus) and high arches (pes cavus).
Physiotherapy management aims to reduce pain, promote accelerated healing and restore normal foot mechanics. Treatment may start with manual therapy with the aim of reducing pain, improving soft tissue mobility and joint function. Stretching of both the plantarfascia and the calf complex (gastrocnemius and soleus) can help also to offload the plantarfascia and improve general soft tissue mobility. Progressive strengthening of the intrinsic and extrinsic foot muscles is also very important when considering rehabilitation. This allows the foot to be strong enough to withstand load such as walking and running without the plantarfascia becoming inflamed. Taping and/or temporary orthotics can also be helpful if foot posture and mechanics are not optimal. Education is a crucial part of physiotherapy management. Understanding the nature of plantarfasciitis, healing timeframes and advice on appropriate footwear are common areas of education.
A multimodal approach to treating plantarfasciitis is recommended as combining manual therapy, strengthening, stretching, and patient education addresses both the symptomatic pain and the underlying biomechanical contributors; leading to improved outcomes compared to one single intervention alone. Evidence supports that integrating manual therapy with exercise and load management produces greater short and medium term improvements in pain and function than isolated treatments (Cleland et al., 2023).
Morton’s Neuroma
Morton’s neuroma is a painful condition caused by irritation or compression of the nerves that sit between the bones of the forefoot/toes (metatarsals/phalanges), most commonly between the third and fourth metatarsal heads. This can result in perineural fibrosis and nerve thickening. This presents clinically as a burning, tingling, or sharp pain in the forefoot.
Common causes of Morton’s neuroma include:
- Tight or high-heeled footwear. This can cause compression and increased load to the forefoot, subsequently irritating particular nerves.
- Similar to plantarfasciitis; repetitive loading such as running and jumping sports.
- Biomechanical abnormalities such as overpronation or bunions.
Physiotherapy focuses on reducing neural irritation and optimising foot mechanics. Interventions may include metatarsal mobilisation and soft tissue release to relieve local compression of the nerve. Metatarsal padding or orthotic inserts to redistribute pressure away from the irritated nerve is also a common form of treatment for neuromas. Advice on footwear modifications is another important element physiotherapists will cover. Shoes that have wider toe boxes and low heels compress the irritated nerve less and thus reducing the potential of further irritation. Strengthening and exercise prescription specific to the foot is useful to strengthen the foot stabilisers and to also correct any faulty biomechanics contributing to pain. Nerve glides and mobilisations are often prescribed alongside exercise to target the effected nerves directly. Early identification and conservative management are essential to prevent progression and reduce the likelihood of requiring invasive interventions such as injections and nerve ablation.
A multimodal approach for Morton’s neuroma, combining manual therapy, foot orthotics, exercise, and load management strategies, can address both nerve irritation and biomechanical contributors, potentially improving pain and function. While evidence is limited and of low value, case reports and systematic reviews suggest that a multimodal approach is more effective than single‑modality treatment alone (Matthews et al., 2019).
Achilles Tendinopathy
The Achilles tendon is the strongest tendon in the body, connecting the calf muscles (gastrocnemius and soleus) to the heel bone (calcaneus). Achilles tendinopathy refers to a spectrum of tendon pathology ranging from reactive inflammation to degenerative changes due to repetitive overload.
Common causes of achilles tendinopathy include:
- Sudden increase in training volume of intensity. This can cause load induced inflammation to the achilles tendon.
- Calf muscle tightness and/or weakness. It is important that these muscles are both strong as well as flexible. Having a deficit here can increase load to the achilles tendon.
- Poor low limb biomechanics such as excessive pronation has been found to increase loading to the tendon.
- Poor footwear and/or training surfaces. Footwear that does not provide adequate support either from wear and tear or from a design aspect can increase loading again to the achilles.
A physiotherapist will first assess the stage and severity of achilles tendinopathy before implementing a graded loading program tailored to the individual. Evidence-based treatment approaches for managing achilles tendinopathy include eccentric or heavy slow resistance exercises to stimulate tendon adaptation. Manual therapy to address surrounding soft tissue and joint stiffness is also utilised. The use of heel lifts or taping to temporarily reduce tendon load can also be beneficial. For chronic cases shockwave therapy may be considered where available and clinically indicated. Education on load management is also essential to help patients balance activity and recovery. Rehabilitation of achilles tendinopathy typically spans several months, with progressive strengthening being a central component for achieving long term recovery and reducing the risk of re-injury.
You should seek assessment from a physiotherapist if you experience persistent or worsening foot pain lasting more than a few days, pain that interferes with walking or activities, swelling, deformity, bruising, or sensations of burning, tingling, or numbness in the foot or toes. Early physiotherapy evaluation enables an accurate diagnosis and timely treatment, helping to reduce the risk of chronic pain, compensatory patterns as a result of pain and most importantly getting you back to doing the tasks that are meaningful to you!
Foot pain, whether arising from plantarfasciitis, Morton’s neuroma, or Achilles tendinopathy, can significantly impact daily function and quality of life if left untreated. Evidence and clinical experience strongly support a multimodal approach to treatment, combining exercise therapy, manual therapy, load management, footwear or orthotic interventions, and patient education to address both symptoms and underlying biomechanical contributors. Physiotherapists play a central role in guiding this process, conducting thorough assessments to determine severity, identifying contributing factors such as muscle imbalances or abnormal foot mechanics, and designing individualised rehabilitation programs. By progressing exercises safely, advising on load management, and implementing supportive interventions like orthotics or taping, physiotherapists help patients reduce pain, restore function, and prevent recurrence. Early professional assessment is particularly important, as timely intervention can minimise chronic pain, compensatory movement patterns, and the potential need for invasive treatments. Ultimately, following a structured, multimodal physiotherapy plan empowers individuals to achieve long-term recovery, regain mobility, and return to the activities they enjoy with confidence and reduced risk of future injury.
References
Cleland, J. A., Mintken, P. E., McDevitt, A., & Smith, M. (2023). Manual physical therapy and exercise versus electrophysical agents and exercise in the management of plantar heel pain: A multicenter randomized clinical trial. Journal of Orthopaedic & Sports Physical Therapy, 53(2), 75–85. https://doi.org/10.2519/jospt.2023.11380
Matthews, B. G., Hurn, S. E., Harding, M. P., Henry, R. A., & Ware, R. S. (2019). The effectiveness of non‑surgical interventions for common plantar digital compressive neuropathy (Morton’s neuroma): A systematic review and meta‑analysis. Journal of Foot and Ankle Research, 12. https://doi.org/10.1186/s13047-019-0320-7
Trojian, T. H., Tucker, A. K., & Scholten, P. (2023). Plantar fasciitis. In StatPearls [Internet]. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK431073/