What is it?
The Achilles tendon is a thick band of tissue that connects the calf complex to the heel bone. It is crucial for walking, running and jumping. This tendon is key for energy storage and release, force transmission, shock absorption and stability, and facilitating that ability to point your foot (plantar flex).
Tendinopathy refers to a failed healing response in a tendon. It results from repetitive stress or overuse of the tendon, with loads exceeding the tendons ability to adapt.
This condition can affect anyone, but certain population groups have a higher chance of developing it, these include post-menopausal women, athletes, and those that are deconditioned.
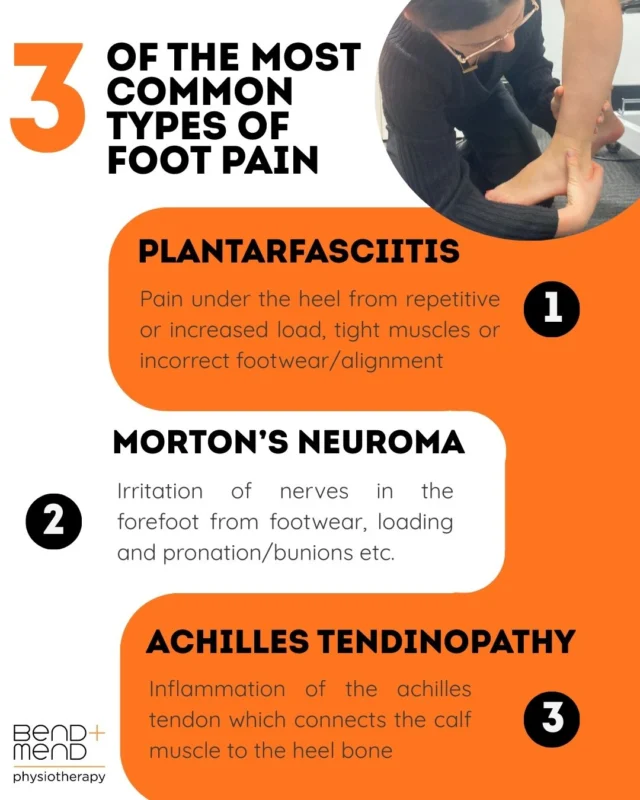
There are 2 locations of achilles tendinopathy:
- Insertional achilles tendinopathy: Affects the lower part of the tendon, close to where the tendon attaches at the heel. While thought to occur exactly at the insertion, it usually affects the area just above, where the tendon is compressed by the heel bone.
*Treatment considerations: avoid compressive stress, such as dorsi-flexion especially in initial stages
- Mid-portion achilles tendinopathy: refers to around 2-7 cm above the insertion of the achilles, where the tendon is most commonly injured.
Why does it happen?
Achilles tendinopathy occurs due to repeated overload. Common contributing factors include:
- A sudden increase in activity (e.g. running or jumping)
- Poor footwear and biomechanics
- Weak calf muscles
- Aging
- Inadequate recovery between training
The tendons are made up of 2 key proteins:
- Type I collagen – provides strength
- Elastin – allows for stretch and recoil
In a healthy tendon, these fibres are aligned and structured. Over time, repetitive loading leads to a thickened, and disorganised tendon that is less efficient at handling stress.
Signs and symptoms
- Morning stiffness and/or after periods of rest
- Pain
- Swelling or visible thickening of the tendon
- Tenderness of the achilles
Stages of tendon change
Tendon injuries exist on a continuum:
- Reactive tendinopathy: early stage is reactive tendinopathy. It’s a short-term response to increased load/stress on the tendon. The tendon cells change in structure slightly.
- Tendon disrepair: The tendon will start to show structural breakdown, i.e. collagen fibres are disorganised but healing potential remains.
- Degenerative tendinopathy: The tendon has undergone long-term damage, reducing its capacity for healing.
More often than not, patients with achilles pain will present in the tendon disrepair or degenerative stage. Despite there being, on a structural level little to no healing potential, physiotherapy is still highly effective.
How Physiotherapy helps
Physiotherapy is an effective treatment for achilles tendinopathy and can help to manage early pain and start the reloading process in a safe manner. We can often restore function, reduce pain and help the tendon adapt to load again.
Key components of treatment include:
- Load management: it is important to stay active, but you may need to adjust or reduce activities that aggravate the tendon
- Exercise therapy: progressive loading exercises are a key component of any tendon-based rehabilitation. You may start with isometric exercises, then advance to eccentric and heavy slow resistance training. The type and dose of these exercises is specific to each individual’s signs, symptoms and goals.
*Note: mild discomfort with exercise is often acceptable, but guidance from a physiotherapist is essential.
- Addressing other factors: these include foot mechanics, gait and training habits
What to do next
If you’re experiencing pain at the back of the ankle, it is worth consulting a Physiotherapist. A tailored rehabilitation can help you return to activity safely and confidently.